(This post is especially relevant to doctors and physiotherapists and others who work with those in chronic pain)
What many physiotherapists and doctors don’t understand about chronic pain
In medical jargon there is the expression kinesiophobia, ‘fear of movement’. I’ve always found this an odd concept. It is said that many chronic pain patients experience a fear of movement because of associating movement with pain. So, the assumption is that they fear pain. Those with chronic pain are, by definition, those who live with the most pain. It doesn’t seem natural to me to talk of fearing something that is already a major part of your life. If you wear a suit to work every day – you may dislike it, sure, but you wouldn’t fear it, would you? You might wear it only when obliged to do so, and wear super-casual clothes the rest of the time i.e. you may well limit your exposure to it, but fearing it would be unusual.
Chronic pain is something only those who experience it can truly understand. It isn’t accurate to think ‘well, I know what pain is, so chronic pain is just having that a lot of the time’ (which those without chronic pain tend to think either sounds awful or not too bad at all). Prior to getting chronic pain I regularly played full-contact rugby. I loved it. I loved tackling people. I didn’t mind the bloody lip, the bruises and feeling a bit battered. Doing this once a week was, however, NOT a taste of chronic pain in any way. Nor was ju-jitsu, or taekwondo, or boxing. Nor was period pain, or toothache, or a headache. The relentlessness (and total pointlessness of the pain) is not possible to imagine until it happens to you.

Imagine you enjoy sitting out in the garden when it’s sunny. One day it’s raining and someone asks you why you’re not sitting in the garden. Er, duh. It’s not much fun in the rain. Do you fear rain? No, it’s just not enjoyable sitting out when it’s raining. So why do some medical professionals really have a problem understanding that people’s preferences change when they live with chronic pain? If anyone wants me to live like I did prior to chronic pain, I want them to sit out in the rain, and enjoy it.
Movement avoidance isn’t necessarily due to fear of harm either
Now imagine you’re someone who enjoys going on walks and also reading. Imagine that you have the option to either read for a while or go for a walk while someone repeatedly stabs you in the neck with a fork, and you can’t stop them. I think I can guess what you’d choose. And what if someone tells you that, although the fork stabbing might be unpleasant, it’s not harmful. You’re still choosing reading, right?
Now what do you think about patients who avoid some pain-inducing activities, choosing to do something else instead?
Only when someone tells you that if you don’t choose the walk you’ll get unfit and get stabbed with a fork during even more activities would you reconsider.
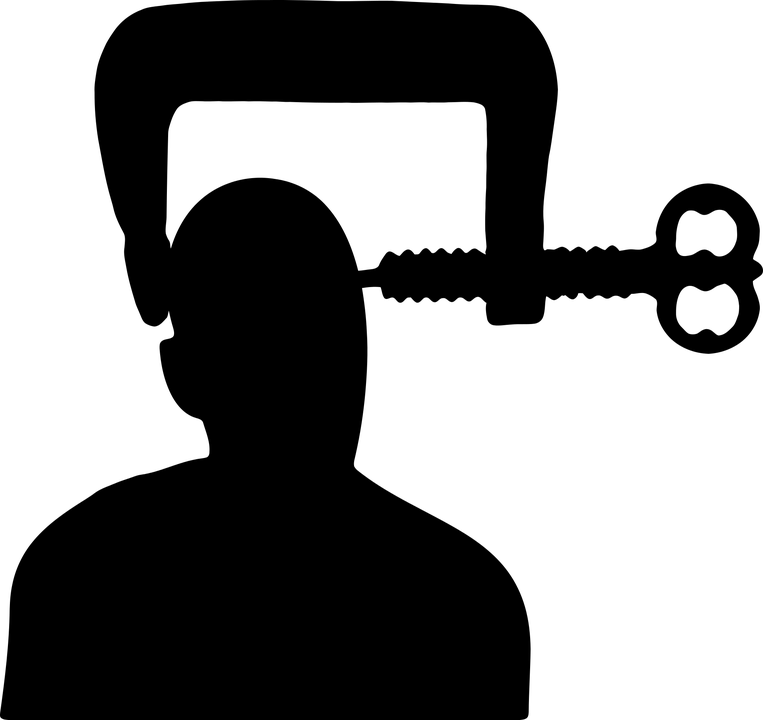
A common belief is that patients avoid movement because they believe pain signifies damage to the body. Well, I’m sure some people do, and it’s certainly right to point out that pain can be completely meaningless and unhelpful, as is often the case with chronic pain.
But that’s not necessarily going to make someone start being as active as they used to be, because some activities are just not appealing any more, or not as appealing as pain-free options. I get headaches watching films, so don’t do it as often as I used to, but have gained a great love for podcasts and audiobooks. I’m not scared of the pain watching a film brings on… I’d just rather do something else.
Of course, what really is an issue and what patients do need to know is that if they avoid all physical activity, they’ll lose muscle tone and may experience more pain in the long run. Knowing this will potentially reduce ‘movement avoidance’ in patients who are motivated by long-term goals; perhaps not so much others.
Also, I’ve come across a few things recently suggesting the role of physiotherapists when dealing with chronic pain patients is to get them moving more. Hmm. Well, if that’s what the patient wants, fine. I’m not totally sure, however, that everyone goes to a physiotherapist wanting to be persuaded to sit out in the rain more, or spend more time getting stabbed with a fork, to continue the metaphors.

More exercise doesn’t always mean less pain long term
As far as I’m aware, it has not been proven that people with all types of chronic pain will be able to get back to their previous level of activity if they do it gradually. I’ve really tried, both with sudden increases in activity and the opposite, gradually increasing walking time by just one minute per month. In neither case did my pain levels decrease and in neither case was I able to keep up the increase, as the increased pain interfered too much with my sleep. I recognise that many people may find that doing more activity builds muscle and enables them to do more with less pain: but it can’t be the case for absolutely everyone.
For me and for many others, limiting movement is about keeping pain levels bearable and being able to work, sleep and enjoy life as much as possible. It’s not always about fear or a poor understanding of pain, or even poor motivation levels. It is a way of coping and it is a pain management system. It might be the best option for some of us, and though exercise-loving physios may struggle to understand, life’s not all about physical activity. Since developing chronic pain, I’ve really enjoyed doing more art, writing, reading and listening to the radio. I do what exercise I can each day, ideally a short walk in my area looking at the nice gardens and the wonderful lake, and sometimes chores and a few all-body exercises. Chronic pain sometimes requires adaptation and change, and perhaps medical professionals should take the time to delve a little deeper into why a patient is avoiding some things, what could help them to do it again, and whether they have found any alternatives.
Related links:
https://stickmancommunications.blogspot.co.uk/2017/01/hypermobility-reluctance-to-exercise.html